TMS for Stroke: A Breakthrough in Post-Stroke Recovery
Stroke is one of the leading causes of long-term disability worldwide. Survivors often face a wide range of physical and cognitive impairments, making rehabilitation a critical part of their recovery. While traditional therapies such as physical therapy, occupational therapy, and speech therapy play vital roles, advancements in neuroscience have opened new doors for treatment. One such promising method is Transcranial Magnetic Stimulation (TMS).
In this blog, we explore how TMS For Stroke can be a game-changer in neurorehabilitation, its mechanisms, benefits, safety, and what patients can expect from this innovative approach.
What Is TMS?
Transcranial Magnetic Stimulation (TMS) is a non-invasive brain stimulation technique that uses magnetic fields to stimulate nerve cells in the brain. TMS has been widely used in the treatment of depression, anxiety, and other mental health disorders. More recently, researchers and clinicians have begun to explore its potential in aiding recovery from neurological events like strokes.
The procedure involves placing a magnetic coil near the scalp. This coil emits repetitive magnetic pulses that target specific areas of the brain responsible for motor control, cognition, and mood regulation. The goal is to rewire the brain and promote neuroplasticity — the brain’s ability to form new connections and pathways.
Understanding Stroke and Its Effects
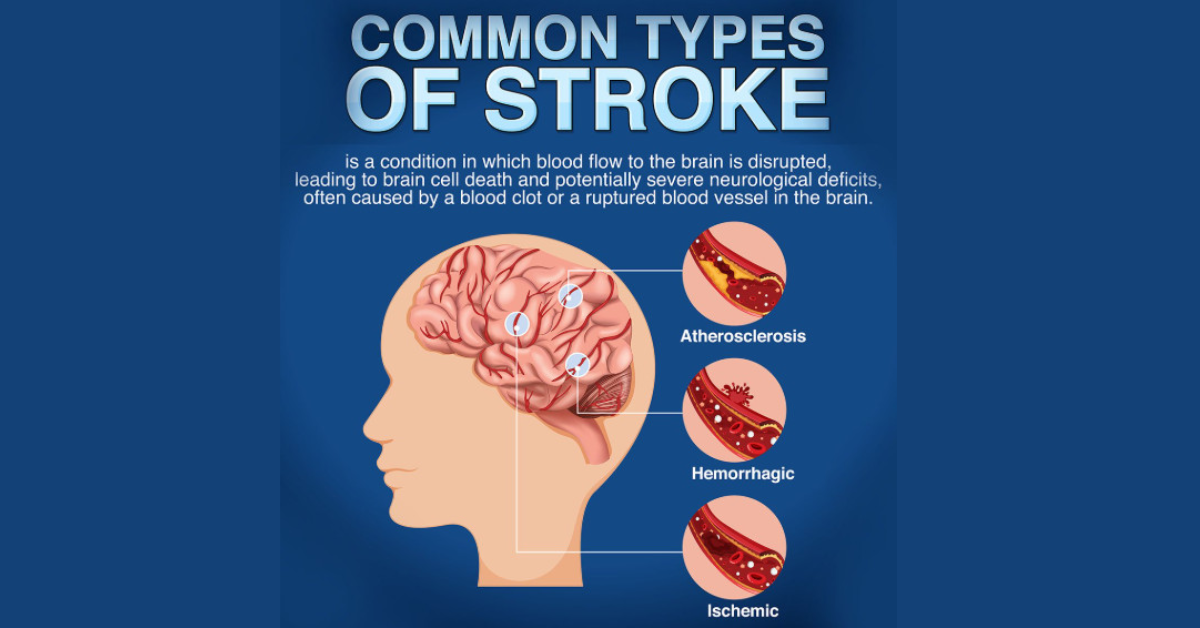
A stroke occurs when the blood supply to a part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. This can lead to brain damage, resulting in various impairments such as:
-
Weakness or paralysis, usually on one side of the body
-
Difficulty speaking or understanding speech
-
Cognitive challenges like memory loss or poor attention
-
Emotional changes, including depression and anxiety
Traditional rehabilitation often focuses on relearning lost skills through repetition and targeted therapy. However, progress can be slow, and many patients are left with residual disabilities. This is where TMS offers a new avenue of hope.
How TMS Helps Stroke Recovery
TMS can enhance stroke recovery by targeting areas of the brain that were either directly affected by the stroke or are compensating for lost function. Here’s how TMS supports the rehabilitation process:
1. Promotes Neuroplasticity
Neuroplasticity is crucial after a stroke, as the brain must find new ways to perform tasks formerly managed by damaged regions. TMS stimulates neuroplastic changes, making the brain more adaptable and responsive to therapy.
2. Reduces Interhemispheric Imbalance
In stroke patients, especially those with motor deficits, the unaffected hemisphere can become overactive and inhibit recovery of the damaged side. TMS can be used to either excite the damaged hemisphere or inhibit the overactive healthy side, thereby restoring balance and improving function.
3. Enhances Motor Recovery
TMS has shown promising results in improving motor function in stroke patients. By targeting the motor cortex, TMS can improve coordination, muscle strength, and control — especially in the hands and arms.
4. Improves Cognitive Function
Strokes often affect cognitive abilities, including attention, memory, and problem-solving. TMS can stimulate brain regions responsible for these functions, aiding cognitive rehabilitation alongside traditional therapies.
5. Alleviates Post-Stroke Depression
Depression is common after a stroke and can hinder recovery. TMS is FDA-approved for treatment-resistant depression and has been effectively used to elevate mood in stroke survivors, thereby improving motivation and participation in rehabilitation.
TMS Procedure: What to Expect
Initial Assessment
Before starting treatment, a comprehensive evaluation is done to determine the patient’s suitability for TMS. This includes medical history, current symptoms, and diagnostic imaging to identify target areas in the brain.
Treatment Sessions
TMS sessions are usually conducted five days a week for four to six weeks. Each session lasts about 20 to 40 minutes. The patient sits comfortably while the TMS coil is placed over their scalp. Magnetic pulses are delivered painlessly, with some patients reporting a tapping sensation.
Customization
The frequency, intensity, and placement of the coil are customized to suit the individual needs of the patient. This ensures maximum efficacy and safety.
Post-Treatment Monitoring
Progress is monitored throughout the treatment. Adjustments may be made depending on the patient’s response. TMS is often combined with physical and cognitive therapies for comprehensive care.
Clinical Evidence Supporting TMS for Stroke
Several clinical studies have demonstrated the efficacy of TMS in aiding stroke rehabilitation. Notably:
-
A study published in The Lancet Neurology found that repetitive TMS (rTMS) significantly improved hand function in patients with chronic stroke.
-
Research from The American Journal of Physical Medicine & Rehabilitation reported improved gait and mobility following TMS treatment in post-stroke patients.
-
Cognitive improvement, particularly in attention and working memory, was noted in stroke survivors treated with TMS in studies conducted by neurorehabilitation centers in Europe and Asia.
These findings suggest that TMS, when used appropriately, can be a powerful tool in enhancing post-stroke recovery.
Safety and Side Effects
TMS is generally well-tolerated and considered safe for most individuals. It is non-invasive, does not require anesthesia, and allows patients to resume daily activities immediately after sessions.
Common Side Effects:
-
Mild scalp discomfort or headache
-
Tingling or twitching of facial muscles during treatment
Rare Side Effects:
-
Seizures (extremely rare and mostly in individuals with a history of epilepsy)
-
Temporary hearing discomfort (if ear protection is not used)
Proper screening and expert supervision greatly reduce the risk of side effects.
Who Can Benefit from TMS After a Stroke?
TMS may be suitable for stroke survivors who:
-
Have persistent motor deficits despite standard therapy
-
Suffer from post-stroke depression
-
Experience cognitive impairments such as memory or attention issues
-
Have stable medical conditions and no history of epilepsy
Not all patients are candidates for TMS. A thorough assessment is necessary to determine eligibility.
Combining TMS With Other Therapies
One of the strengths of TMS is its ability to complement existing rehabilitation strategies. When combined with:
-
Physical therapy, it can enhance motor recovery.
-
Speech therapy, it may support language improvements in aphasia.
-
Occupational therapy, it can accelerate regaining daily life skills.
This integrative approach leads to a more holistic and effective recovery plan.
The Future of TMS in Stroke Rehabilitation
As research continues, the potential applications of TMS in neurorehabilitation are expanding. Advanced imaging and AI-driven protocols are making it possible to personalize treatments more precisely. In the future, we may see TMS integrated into home-based neurorehabilitation systems or used in combination with virtual reality and robotics.
FAQs About TMS for Stroke
1. Is TMS FDA-approved for stroke treatment?
While TMS is FDA-approved for depression and other mental health conditions, its use in stroke rehabilitation is considered off-label. However, it is supported by a growing body of scientific research and used in many advanced rehabilitation centers.
2. How soon after a stroke can TMS be started?
TMS can be introduced as early as a few weeks post-stroke in certain cases, but many providers begin TMS during the subacute (1–6 months) or chronic phases of recovery. Timing depends on individual clinical factors.
3. How long does it take to see results from TMS?
Some patients begin to notice improvements after a few sessions, while others may require several weeks. Consistency and integration with other therapies enhance outcomes.
4. Can TMS be repeated if needed?
Yes, TMS can be repeated if symptoms persist or if the patient benefits from periodic maintenance sessions. The treatment plan should be guided by clinical evaluation.
5. Are there any age limits for using TMS after a stroke?
TMS has been used successfully in both younger and older adults. However, elderly patients should be carefully evaluated for suitability, especially if they have other health conditions.
Conclusion
TMS for stroke represents a new frontier in neurorehabilitation. By harnessing the brain’s plasticity and providing targeted stimulation, TMS offers a non-invasive, safe, and potentially transformative approach to recovery. While it is not a standalone solution, when combined with traditional rehabilitation therapies, it can significantly improve quality of life and functional outcomes for stroke survivors.
For those exploring advanced options for stroke recovery, TMS may be worth considering under the guidance of trained professionals. As the science evolves, so does the promise of helping patients regain more of what was lost — and perhaps even achieve outcomes once thought impossible.